Colon and rectal growths are often silent but can carry serious health risks if left undetected. These growths—ranging from harmless polyps to potentially deadly colorectal cancer—typically begin in the inner lining of the large intestine or rectum. The good news? Early detection and proper care can significantly improve outcomes.
🧠 What Are Colon & Rectal Growths?
Colon and rectal growths refer to abnormal tissue that forms in the colon (large intestine) or rectum. These include:
- Polyps – Small, often benign clumps of cells. Some types (like adenomatous polyps) can turn into cancer.
- Benign tumors – Non-cancerous growths that usually don’t spread.
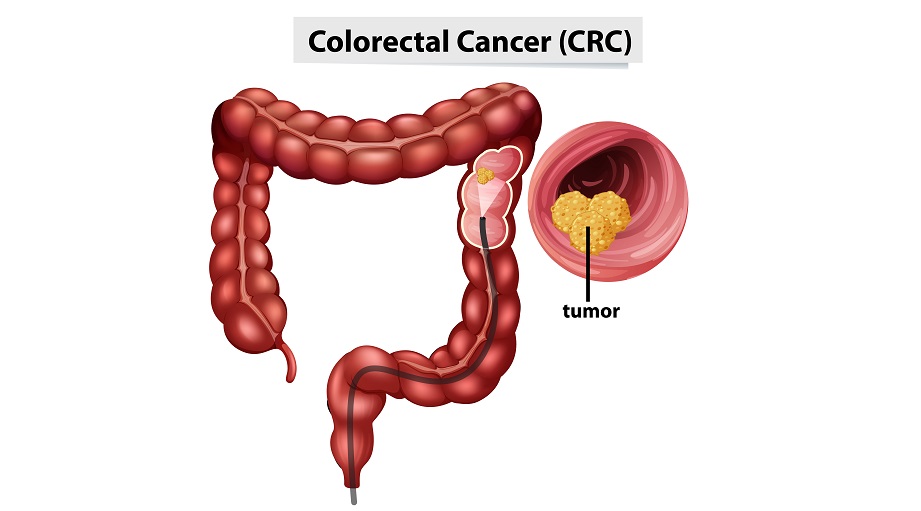
- Malignant tumors – Cancerous growths that can invade surrounding tissue or spread to other organs (colorectal cancer).
🔍 Common Causes & Risk Factors
The exact cause of these growths isn’t always clear, but several factors increase risk:
- Age – Most common after 50
- Family history of colorectal cancer or polyps
- Inflammatory bowel disease (IBD) like Crohn’s or ulcerative colitis
- Sedentary lifestyle
- High-fat, low-fiber diet
- Smoking and alcohol
- Obesity and diabetes
- Genetic syndromes such as Lynch syndrome or FAP (Familial Adenomatous Polyposis)
⚠️ Symptoms to Watch Out For
In many cases, early-stage polyps and cancer may not cause symptoms. But as growths progress, signs may include:
- Blood in stool or rectal bleeding
- Changes in bowel habits (diarrhea, constipation, or narrowing of stool)
- Persistent abdominal pain, cramping, or bloating
- Unexplained weight loss
- Feeling that the bowel doesn’t empty completely
- Fatigue or signs of anemia (pale skin, shortness of breath)
If you experience any of these symptoms for more than a few days, consult a doctor right away.
🧪 How Are They Diagnosed?
Detecting colon and rectal growths involves:
- Colonoscopy – A camera is used to view the colon and remove or biopsy polyps.
- Sigmoidoscopy – Examines the lower part of the colon.
- Stool tests – Detect blood or cancer-related DNA.
- CT colonography (virtual colonoscopy) – A non-invasive scan to check for growths.
- Biopsy – Determines if a growth is benign or malignant.
🩺 Treatment & Management
Treatment depends on the type and stage of the growth:
- Polyp removal – Done during colonoscopy to prevent cancer.
- Surgery – For larger or cancerous tumors.
- Chemotherapy or radiation therapy – For advanced colorectal cancers.
- Targeted therapy – In some cases of metastatic cancer.
- Lifestyle changes – Diet, physical activity, and smoking cessation are key to prevention.
⏰ When to See a Doctor
You should seek medical attention if you:
- Notice blood in your stool
- Experience persistent changes in bowel habits
- Have a family history of colorectal cancer or polyps
- Are over 45 and haven’t had a colonoscopy yet
Early screening can detect and remove polyps before they turn into cancer.
❓ FAQs
Are all colon polyps cancerous?
No. Most are benign, but certain types can become cancer over time.
Can colon cancer be cured?
Yes—especially if found early. That’s why screening is crucial.
Is colonoscopy painful?
It’s usually done under mild sedation and is not painful.
How often should I get screened?
Typically every 10 years after age 45, but more frequently if you have risk factors.
✅ Final Thoughts
Colon and rectal growths might seem minor, but they can develop into something more serious if ignored. Regular screening, especially after age 45, and a healthy lifestyle are powerful tools in preventing colorectal cancer. Don’t delay—early detection saves lives.
Colon polyps, rectal growths, colorectal cancer symptoms, blood in stool, colonoscopy, bowel cancer, large intestine tumor, colorectal cancer risk, colon polyp removal, GI doctor
